
Gain expert insights into the TEAM Model’s purpose, design, objectives and more!
Get your free copy of TEAM: The new mandatory CMS model replacing CJR
Conquer CMMI’s episode-based bundled payment model
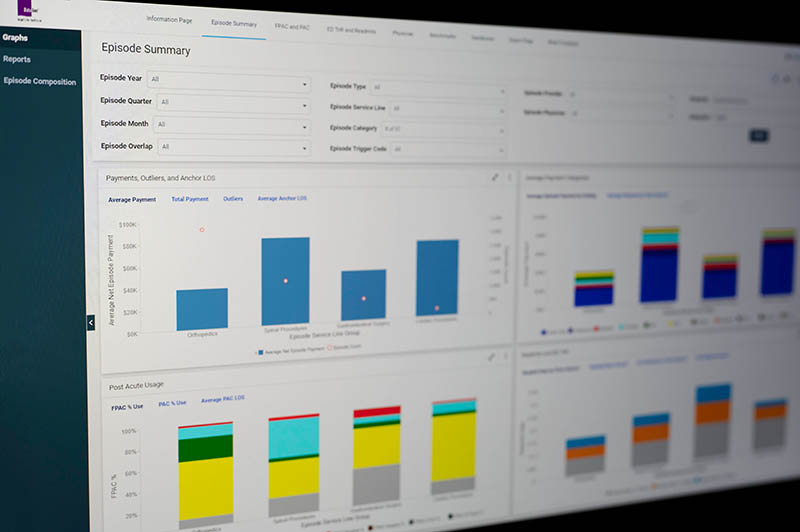
Your acute care hospital needs technical claims knowledge and data expertise to get ahead of complex Medicare payment policies. DataGen provides you with the tools to successfully navigate the Transforming Episode Accountability Model (TEAM) payment methodology. Access essential analysis services that help you conquer CMMI episode-based payments, including
- baseline opportunity analysis;
- performance data monitoring; and
- reconciliation validation.
Make CMS TEAM Model preparation an easy lift
Say goodbye to cumbersome file manipulation and hours spent reading the Federal Register. Empower your decision-making processes with critical Medicare bundle payment data:
- identify cost drivers that create differences in Medicare episode spend;
- understand utilization patterns over time and compare to benchmarks;
- conduct “what-if” analyses to understand potential opportunities to create savings; and
- validate CMS’ reconciliation calculations when the model is live.


High-touch value-based care assistance
DataGen has more than a decade of experience working with providers that participate in Medicare alternative payment models. We make it easy for you to get the right information at your fingertips so you can focus on what matters — practice transformation. Start feeling empowered with your data and get a head start for proposed mandatory CMS TEAM Model participation.
Boost your analytics to achieve clinical, quality and financial goals.
Explore our Transforming Episodes Accountability Model (TEAM) solutions today!

Frequently Asked Questions
-
What problem does this solution solve under TEAM?
TEAM requires hospitals to enhance care coordination and manage Medicare episode spend in comparison to a regional target price. Our solution gives you visibility into episode risks and opportunities, potential financial exposure and ongoing performance monitoring so you can improve care delivery before results are final.
-
What data does the platform use?
The platform leverages two data sources:
- your hospital’s CMS TEAM episodes, claims and target price files; and
- benchmarks created by DataGen using national Medicare fee-for-service datasets.
DataGen applies Medicare’s payment policy rules and CMS TEAM specifications for episode-based payment evaluation and reconciliation forecasting.
-
Can this help us manage post-acute care costs?
Yes. It is essential to understand post-acute care utilization in the episodes of care included in CMS TEAM. Our solution provides insight into which post-acute care providers are being used along with important indicators such as episode volume, Medicare spend per episode, length of stay, rehospitalization rates and Medicare Star Ratings.
-
Are there benchmarks that we can compare performance to?
Yes. DataGen simulates TEAM episodes of care according to CMS’ specifications for every hospital in the country using national Medicare datasets to provide hospitals benchmarks to compare their performance. Comparative groups include region, academic medical centers, hospitals of similar bed size, top performers and more. Not only do benchmarks provide hospitals with an idea of what utilization/performance is possible, they also help hospitals estimate potential savings based on changes in care delivery.
-
How early can we see reconciliation results?
Our solution uses monthly episodes and claims data updates that CMS makes available to hospital participants and is updated within days of release. Although all claims received to date are included for performance monitoring purposes, we consider episodes to be complete for financial analyses 90 days after the episode end date, allowing for necessary claims data run-out to occur.
In addition, our solution recalculates the CMS TEAM target price according to your hospital’s patient case mix in the performance year, providing more accurate target prices for comparisons ahead of CMS’ release of reconciliation results. This helps hospitals see projected reconciliation outcomes throughout the performance year, allowing clinical, financial and care management teams to act sooner.
Note that the official CMS TEAM reconciliation results for a given performance year will not be available until six to nine months after the end of the performance year.
-
How does this support cross-functional teams?
The platform is built for finance, care management and strategy teams alike, providing a shared, defensible view of episode performance that supports faster, better-aligned decision-making.
-
How long does implementation take?
Implementation is streamlined to support TEAM timelines, with a focus on getting actionable insights in front of teams as quickly as possible (not months down the road). As long as your hospital has completed all required documentation with CMS to gain access to your CMS TEAM data, our solution can be implemented within days of receiving your hospital’s data.
Contact
Leave your name and email and we’ll be in touch! Reach out to:
- access a free demonstration of our product analyses and data platforms;
- meet our team of healthcare data and policy experts devoted to your success; and
- optimize your workflows and cut out unnecessary tasks.











